The transplant program at Duke has really taken off, and to be quite honest, it is outgrowing the large facility; oxygen equipment and the room to store it in, classroom space that now requires splitting up the groups and caregivers; waiting for equipment to free up. It’s usually not too long of a wait for anything – but there are some times that are less crowded than others. While we were on the floor, a white board has been set up with three groups identified: Walk, Weights and Bike. Each category has 15 or so names listed. The group has been split up into exercise stations that we will rotate through in a clockwise manner. Meanwhile… the graduate group is already at the stations working their way thru, so the next hour will be a bit congested with the two groups overlapping.
As people who know me know…I don’t like being crowded. Closeness with others makes me uncomfortable. Not because I am bashful, or think I am better than anyone, but because I just get overwhelmed with a sensation…like a claustrophobic type anxiety. I don’t like shopping malls, church dinners at group tables, crowded festivals and events or any activity in a group that becomes too crowded. I NEED my space. This will probably do me good in the future when my immunity suppression is in place making me more susceptible to germs, fungi and bacteria. It’s not that I don’t enjoy talking with other people, but I want the openness of space around me…so I tend to sit apart from the crowd. I also tend to be more of a listener and observer than a talker and doer…that is until I am “on-stage”. I love to educate and share information in a structured setting. Therefore, over the years I have made my times alone, even in a crowd, a time of “learning”. I really do like being a people watcher and behaviorist. It’s the “Harriett the Spy” in me.
I have noticed something universal in this new life. There is one very obvious thing that tends to separate and reveal the pre-transplant people from the post-transplant people. And interestingly enough – it is conversation during our workout day. The pre-tx folks are so busy just trying to breathe, they don’t have the breath to chatter with those sitting or
walking next to them. Many of the ones who have received new lungs are always talking,,,they hardly stop. It was probably in their make-up to be that way anyway...but it si charmingly interesting to watch them pair up and chatter away, unencumbered by shortness of breath.
(Very good observation. My parents would ask me to stop talking after transplant. They were only kidding of course but I just would not stop talking. It was like I was making up for lost time. Just having the energy to talk is a true blessing!) It can be irritating sometimes too though. When the trainers microphone stops working and the “talkers” laying on mats next to each just other keep talking… it’s hard enough to follow the instructions, and sort out the trainer’s muffled voice from all the machines whirring and churning all around us, without having to sort through all the gabbing going on. And when it happens on the track, it causes traffic jams because the talkers block and restrict two or three lanes as they walk side by side which only leaves one for the rest of the pack to single file through. It’s like a log jam on a plume as walkers single file wait for their chance to wiggle by. The pre-transplantees don’t have energy or air to waste on conversation. They save it for when the break times come, before and after sessions, when we slip back into our chairs and knock the oxygen levels back to our resting numbers. So even though the masks and cannulas, or lack of cannula, give the 2 populations away visually, the behavior differences between the two groups is prominently evident. I will be watching to see how this dynamic interaction changes as more of my group gets their transplant and make their way back to the group for post tx rehab. Who then will be the talkers…and who will be the walkers? Should be interesting to see if my observations and guesses prove right.
Always thinking…
Each day we are rotated to start at a different station. So, if I started at the weights today, then tomorrow I’ll start at bikes and the next day my starting activity will be walking. It breaks up the monotony that way. Another help in breaking up the routine is by alternately walking counter-clockwise around the track one day and switching to clockwise the next. If the group I am assigned to is walking, then first we must report in to the trainer desk.
They verify that our tanks have sufficient oxygen in them to get us around track for our duration; if it is set to the proper oxygen level, and if we have our counting beads with us. On our first day we were presented with a cord of approximately 30 little plastic colored beads strung on. I tried using them a day or two. But I found them too small and easy to miscount with. I bought me some larger wooden beads with substance of varying textures, sizes and color tones and made my own counting beads. The trainers set a timer for 20 minutes, unless it is Tues or Thurs, and then we have to walk for 30 minutes. Ugh! I remember my first Tuesday walk…. I thought I would collapse before those 30 minutes were over – but the good news was… I had walked a mile and a half in 30 minutes – or 19 beads (laps).
Walking around and around can get really to be a drudge, particularly for an outside visually oriented person like me, but I try to entertain myself with creative past-times. I noticed a large luna moth dangling on the outside of the window one day, so each time I passed, I focused on looking at it. Each lap the moth became the visual target. Other times, if my caregiver husband was there early for a class and seated in the classroom, I would see him with every pass of the doorway I made, so I started entertaining both of us with smooches blown in his direction…next trip around was a curtsy…next trip was three jumping jacks, or I might throw him an “I love you” in sign language ala gang style etc. I would have a whole lap to think about what my next antic would be and then spring it on him, which helped pass the laps away!
I'm sure I'm not responsible for it in its entirety, but I do know I have been a major contributor to the T-Shirt entertainment circle. There is nothing more fun than to walk the track loop and wait to see what the next T-Shirt says. I try to make each day special as I carefully select a shirt from my immense supply of interesting and unusual T-Shirts. Most I have purchased during vacations, from organizations I supported, from my church or because they would serve as a memory of a special time I had. I love to see what kinds of unusual shirts I can come up with. I have some about trees, trails, rivers and lakes, some about Yogi, Smokey and Capt Kangaroo, Squirrels who are wanted, Bears who are wanted, and wolfs who aren't wanted by many, and of books that I always want. I have cop related shirts, Cartoon Characters and Scenic locations. So far I have only one shirt style from my church, but it was two different colors with the same words. I am seriously thinking about reviving my "Charlie" hats too. Thank goodness I live close enough to haul my collection of shirts back and forth. What will I do during Post Surgery Rehab? Start the rotation all over. Shucks no! I have a whole ‘nother box of T-shirts I have outgrown because of this disease. After surgery, at least for a little while, I will have likely lost enough weight to fit all my Size Small shirts again. Lots of Geocaching and Hiking t-shirt garments to come! I can't wait to bring them all to life again! I love casual work-out garb! LOL
Uh-oh! Problem alert! Someone on the treadmills is wearing strong cologne or body spray. Unfortunately he has positioned himself directly under a rotating fan so that it sends the chemicals in a broad swipe across the track. I can already feel my eyes itching and my airways closing up and I reach for my rescue inhaler. I realize that those who don’t have allergies or breathing problems don’t realize the serious health effects that many perfumes create. It isn’t all perfumes – just ones that use certain synthetic chemicals that compromise our lungs and airways. The reaction is frightening as I begin to gasp for more oxygen to try and balance out the danger of increased shortness of breath. I try to steer myself to the lanes farthest from the poison that attacks me. When I hear people tell me about their headaches and allergies, I wonder if the fragrances they are wearing may just be the very culprit for their own discomfort. I have had to leave businesses, restaurants, doctor’s offices and locations where someone’s chemical fragrance is permeating the room. And large gatherings where folks tend to dress up often present challenges for me such as concerts, church, theater, etc. I had truly hoped the signs that ask for a fragrant free environment might be accepted. If you know there are people who suffer, why would you not? This is twice this man has come into the gym with a strong fragrance on. I have asked for help from staff – but if it happens a third time, I will pray and then approach him myself and ask for his help. I know some may not understand my cries for help, but like I said about helping others through doors, after my surgery, I will never EVER wear cologne again. That is a pretty strong statement from someone who once sold Avon and always wore cologne, but… I have suffered the migraines, the itchy eyes, the swelling of my throat, the uncontrolled coughing. Moving right along…
Some days I would sing songs in my head and wish I had a radio with headphones or knew someone who could teach me to use one of those mp3 thing a ma jigs. I know I am too cheap to wanna buy songs to download, so I daydreamed about burning some of my own CDs instead. After one of my fellow patients had a visit from a rabbi, I got to thinking about other religions. The Greeks use worry beads and Catholics use their beads to do their hail Marys. I have no idea what or how that works, but why not create my own religious application. I decided I would start a lap and pray for a specific person or subject of concern or praise for the entire lap. Now the mind is an interesting thing. It is pretty darn hard to stay focused on one subject for that long of a time without wandering. So this became more of a meandering conversation time with God instead of a traditional prayer. It’s probably the way God wants his children to approach him anyway. So, talk I do, mentally at least,
no breath wasted…as often as possible. I wish I could say I was totally consistent with that for every lap, but I can do better. I’m still thinking about getting those contemporary praise songs. I might have a bit more high step with songs to help me get through the walk. I DO love music.
I have discovered that relationships are being developed amongst the candidates and their caregivers. We are each other’s biggest fans and supporters. Every group is unique unto its own entity based on its’ individual evolving make up. Our current group has an active blog that is updated daily, thanks to a willing volunteer caregiver. It shares information about who was listed, got the call, is in ICU or step-down, heading back to rehab, and unfortunately who didn’t make it and died. We are all very anxious to hear the local news amongst our peeps. It is a really interesting dynamic unfolding as people come and go, have tests and hospitalizations. There is always a warm welcome and sincere happiness of learning about those whose lives are becoming better. That camaraderie carries over into our workouts. It is rare to walk a lap and not see smiling faces encouraging me along the way to keep going. I find myself crawling out from behind my wall to thank someone for their encouragement and to give the same boost of encouragement to someone I see growing weary. It only takes a moment of my time, but can provide all the difference to someone struggling. There is no question that some lifelong friendships are being made at the Center For Living.
I have discovered that there really is a transition that takes place with the body when it is being pushed hard. Some call it endorphins kicking in. Some say it’s a “runner’s high”, some call it getting their “second wind”. Whatever it is, I know it is real. There are times when I am dragging butt and counting the minutes (or beads) for it to be over. And before I know it, a little over half way done, a physiological transition takes place. It suddenly doesn’t seem so hard as it did just a few minutes earlier. The breathing, though labored, doesn’t seem quite as difficult. An energy boost takes place and I realize “Hey, this isn’t quite as bad as I thought it would be”. Whatever it is…I still wait to see that smiling face with a clipboard in hand staring directly at me! Whooo hoo! Black horse and a cherry tree! My time has come! I’m gonna be called in. Hip, hip hooray! Nothing compares to that trainer’s “look” and the subsequent sense of relief which follows. That is probably the one time in my day that I smile my most sincerest smile. I fight a slight muscle disorder in my face that causes one eye to partially close and one side of my mouth to relax into a droop. When I am relaxed or tired, I look like I am frowning. Mama’s face did this…and thanks to my overbite, so does mine. I tend to smile more one sided – but I can override those lopsided jowls of age with a tad bit more muscle effort. The trainer’s signal into the pit stop is always the best initiative I know these days! I count my beads and stick up my index finger for my 02 readings and promptly collapse in my chair to recover.

Next stop is the weight section and I don’t mean Biggest Loser weigh-in. It’s power lift time! There we will alternate days between working on our upper body and lower body. The physical therapist has evaluated our abilities and developed a weights plan to gradually build our strength up. We have about 4-5 different machines for upper body and 4 more challenges such as lifting hand weights, a cane, squats, etc. The next day involves much of the same designed for our specific lower body needs. We stretch all the muscles in our legs which is one of my favorite parts because I can look
outside the window at the woods, birds and skies. I have to also stretch my hips which have been under arthritic attack for the past 8 years…and walk up and down stairs, stretch and strengthen other leg muscle groups. I have very strong legs so I tend to do a few more reps then asked to do, however, this my third week. No two plans are the same. We all have our own individual starting weights and reps to do.
I am finally reaching the point where it is getting harder to do. I enjoy pushing myself. I know I am an over- achiever, but I had a lot of base strength that was wasting away; it has been responding quite nicely this month. I am pleased. I’m also glad to see how good of shape I really am in. I’ve impressed myself, to say the least. I know I wouldn’t have pushed myself quite this hard at home, and they haven’t pushed me too hard either. I have to find that balance where I slow down and let the muscles do things right. I recognize this and know I have finally reached that point. Now I will be listening more to my body so I don’t get hurt. I proved to myself I can handle this as well as I ever did…and now I have to admit that I am sick…and not to push too far. It is a process…a balance. And I am right where I am supposed to be right now. I KNOW I am strong enough for surgery and an excellent recovery. I have made it my priority to achieve this and I am satisfied that I have done it. Now, I just need to maintain it. I don’t have to prove anything…until it is finished! ;-)
I usually don’t need a recovery rest after weights. I just swing by my seat long enough to grab a few more swigs of water and maybe a bathroom break and then off to find myself a bike. We call them bikes, but they are actually something called Nu-Step. We are seated in a recumbent position. Just like sitting in a car. Our feet are extended onto foot pads. Instead of rotating our feet in circular motion like a bicycle does, we use stepping motions to apply pressure on the mechanism that measures our distance, level of resistance, time, watts produces, steps taken, etc. There are also two handles that some people use to help strengthen the arms and assist with the force requirements. We do this for 20 minutes. I used one of these at Morehead Memorial Rehab so I was quite ready to start this my first day at Duke. I already knew how to set it up for my own personal settings…but the one thing I didn’t count on was the way Duke wanted me to use them – with my feet only. No hands to help supply some of the energy needed for rotations. This meant my legs had to do all the work. Although they started me out fairly low, it was no time before I was put on level 4 for 20 minutes. Next comes level 5…..yowza! I am dreading that! I have no idea where I will be next week. Thank goodness I have hit day 17. Only 6 more days before I graduate. It can’t be too much harder! I’ve gotta admit, wiping off equipment is not one of my most favorite parts of the day. The bleach wipes are very strong and irritate my eyes and airways. I try to get it over as quickly as possible, but if I am already having a bad breathing day, I will ask a staff member to help me and do it. They are always quite helpful that way.
I hate to ask someone to do something for me, but I have learned the hard way I have to admit I need help – or suffer the consequences. This disease has made me dependent on others…not somewhere I ever thought I would be. And it is going to get worse once I get “The Call”. It is a humbling time. I take nothing for granted. I feel very, very blessed that I have been offered this opportunity of healing and pray that God continues to strengthen me as I strive to do all I can to overcome this time of trouble.
Speaking of asking for help…there is a group of people who are actually our unsung heroes. They are our caregivers!
These people care enough about us to place their own lives on hold in order to support us. They have to be strong for us. They must make sacrifices for us: willing to move away from home, family and friends, they will be asked to provide care for us, coordinate our days, drive us to and from the Center for Living, to doctor appointments, attend lectures, go shopping, carry our heavy loads, do laundry, clean up behind us, and then….sit and wait. Caregivers need strong emotional health and nerves of steel in order to put up with the stress and moodiness of their patients. They must be patient and forgiving. Since I am still in the pre-lung status - I can’t add all the additional chores they will be required to perform after our surgery, but I do know they will be our nurses; changing bandages, organizing our pills, injecting medication, using feeding tubes, and above all…worry about us. My husband Danny is here in Durham with me and I would be lost without his love and support. He IS my hero. Without him, I would not be able to be here. Yes, our caregivers are responsible for us; what an incredible commitment and selfless giving act of kindness they are making to help us become well again. God bless the caregiver!!
(God bless the caregivers, especially my mom. She had to go through this with my dad 10 years ago next month and this past May with me.)
Another support system that becomes very important to us is our friends and family from home. What would we do without the prayers and well-wishes from them. The transplant team even states the importance of their involvement in achieving motivation for compliance and healing. Every day I find myself in gratitude for my loved ones as I receive cards, emails, Facebook comments full of encouragement and support. Each friend reaching out in sincerity brings a broad smile to me and helps me stay strong. Thanks everyone for your gifts of encouragement!
Okay, so I’ve done all three sections. It’s almost time to go home, that is, unless we have a lecture. Duke has really gotten their act together. Transplant Team members, of all professional walks, come and present lectures to help educate thepatients.
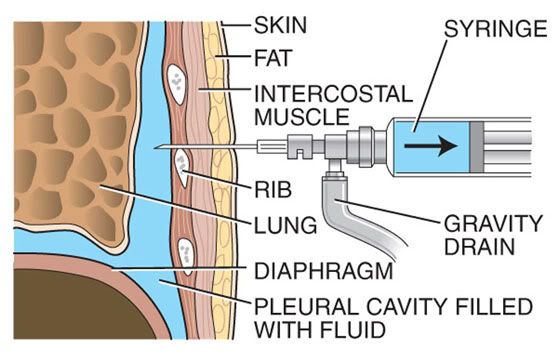
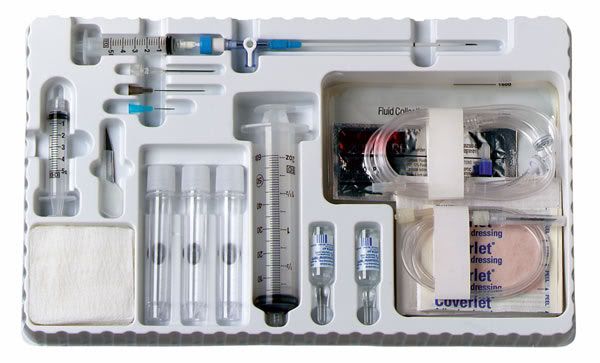
I have spent a great deal of time these past couple of years reading research notes and articles about COPD and Lung Transplants, but the specifics of how things happen were still a mystery to me. Through these classes, we are being shown different phases of what we will see, hear, feel, encounter as well as some of the more difficult subjects to hear…like what could go wrong. We don’t want to dwell on them… but if after transplant we require having tubes stuck in our bellies and intestines for feeding purposes, or a tracheotomy to help us keep our lungs inflated and breathe stronger, then we – patients and caregivers – won’t be so scared and startled when a nurse or doctor informs us of the need. A lot of unnecessary anxiety is being reversed through the exposure of these lectures. As a public educator, I am very appreciative of this style of preparing patients. A more informed camper is a safer and happier camper.
There are lectures designed for pre-tx patients and post-tx, as well as for caregivers. Classroom space prevents us from being together with our caregiver for lectures, which I find a bit unnerving because my caregiver is missing out on some of the stuff I am learning. So, I started carrying a recorder with me and bringing back the handouts so we can discuss them together. I feel bad for those who can’t share with theirs. There is just TOO much information to try to remember and talk about later. I also realize that there is probably another reason they split us and that is to give each group the info they need. Caregivers have to be prepared for the irritable patient and the psychological approach to these medical treatments whereas the patient is medicated and probably couldn’t really give a damn while they are under morphine – until they see the procedural evidence in a mirror later~ 100 staples, or however many there are, can be enough to make anyone irritable. LOL
These are the lecture topics we’ve had to attend (and I thought it was bad at work!) :
What to Expect During Transplant
Meds
Transplant School
Anatomy & Physiology - Parts 1 and 11
Tube Feeding
Oxygen Therapy
Scar Mobilization
Diabetes
Osteoporosis
Speech Therapy
Caregivers Support
Phew. Are you tired yet?????
So, now the day is done. In leaving, steps are reversed. We swap out our oxygen tanks, toss our dirty towels in the bins, peel off our gloves which are literally dripping wet with sweat, gather up our personal lunchboxes, belongings and make our way back to our vehicles or wait for our ride. Since I preplanned my departure, knowing I’d be hot and tired, the walk down hill to a car parked in the shade is almost enjoyable. I know in just a few minutes the air will be cool and I will be pulling up in front of my apartment. I will be hungry, ready to eat and most likely it won’t be too long before I fall asleep.
The first couple of weeks at the Center for Living were pretty rough for me. I was doing some traveling back and forth on weekends or spending time with loved ones, when really I just needed to rest up from this new strenuous activity. My PT time is a full job that I have to plan and prepare for daily with diet, rest, medication and energy. This is above the normal tasks of eating, cleaning, and entertainment. I have to plan my days carefully, when and where I eat, how much, when to take my medicine, what to do when things go wrong…like insomnia. I guess the change of location, unfamiliar surroundings, new routines, exercise energy requirements were really shaking me up hard. I fought hard physically and was mentally drained. I was becoming overwhelmed. My brain was racing around with thoughts trying to absorb the new environment, things we were being exposed to and demanding schedule. Ultimately I had to ask for some medical intervention…and for those who remember…it’s not quite like I “take Sominex tonight and sleep” – it’s better! I don’t feel drugged…or tired but I get the sleep I need! I am very grateful to the medical team and to our coordinators, who keep us going through this process.
Being a major surgical candidate is no light event… like perhaps having a knee operated on… or having a neck operation.
Oh, don’t get me wrong. I don’t make light of either of those procedures. But those of us undergoing a transplant are not having a surgery that will ultimately heal and be better and forgotten because it makes us well. Nope. We will still be sick after transplant. It will be a different kind of “sick” – and we are only beginning to face the challenges that will continue the rest of our lives. We don’t just wait for our scars to heal and then we can breathe, as if nothing ever happened.
Oh, yeah, there will be glorious breath…. lungs filling with air, supplying our bodies with the oxygen it needs.No more oxygen tanks…no more coughing spells, no more suffocation. But rejection is always just right around the corner…it’s mask of death peeping thru the curtain. The lifetime of medication, other subsequent health problems that may accompany our new world, like diabetes, kidney disease, steroid ballooning, are ever-present. Having regular bronchoscopies, taking our weight, temperature, blood pressure and spirometers every day, the added care needed to protect our new lungs from
illness, debris, fungus…will always be crying out to us. There will never be fully any true time of rest. All we have done is postponed the inevitable. We hope that future patients might benefit from the research that is done through our journey. We cling to the time we have been granted to learn the true meanings of life and
we struggle with the knowledge of mortality.
The scars may be healed, but the “gift of life” is on a clock that is ticking. This gift’s original owner has already gone on ahead of us, and it is only time before we too will be reunited with our donor. I know fear will come to many of my peers after surgery and they will live their post-transplant lives in the shadow of that fear.
I choose to live my life looking forward to the future. I have a future here on earth…but I also have a future after life as we know it. I love the thought of being able to climb mountains again, and travel to visit family and play with children in the woods. But I also look forward to being united with Christ, without whom I would not have this hope.
I cannot fathom how people who have no strong family support and faith in God ever make it through this medical process. The stress has to be awful; the unknown, overwhelming. I am so fortunate to be loved by God. I am amazingly calm, at peace and ready to follow these medical people through this process. The hand of the Lord is upon His servant and I believe that with every portion of my being. Healing miracles by God come in many forms, including the hands of surgeons that He grants blessings upon and through. I have been walking in the valley of death for several years now… but I will receive new life. Whether that life will be here on earth or in heaven with Christ, I know that His plan for my life will be fulfilled.
I am humble and sincere when I beg Him to use me in whatever means necessary in the remainder of my life to achieve His plans. I trust Him with my life… with the very breath that He first breathed into my nostrils over 55 years ago. To Him be the glory…forever and ever, amen. And I hope I can shout that from the mountaintops, or at His feet…it makes no difference to me!
Susan Traxel Martin
(For my mother, on this date of August 25, 2011, which would have been her 90th birthday)